Every Year, 8 th May is celebrated for awareness of Thalassemia, genetic disorder. This year International Thalassemia Day’s theme is “Be aware, share, care – Strengthening Education to bridge the thalassemia care gap.” This initiative enables to enable us to educate and spread awareness amongst society about thalassemia and measures to prevent this disease. There are 270 million thalassemia patient in this world. INDIA has highest number of thalassemia patient in the world , INDIA has approx 1 to 1.5 lac patient and about 10,000-15,000 children having thalassemia major born every year.
What is Thalassemia?
Thalassemia is genetic disorder which causes ineffective erythropoiesis meaning body produces an inadequate amount of haemoglobin. Haemoglobin is a protein molecule that has oxygen in the red blood cells. It results in the extreme destruction of red blood cells that leads to anaemia. Anaemia is a condition in which the haemoglobin or red blood cells are less than the regular count.
There are three types of thalassaemia — minor, major and intermedia.
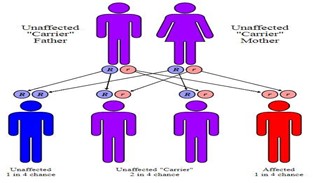
A person with thalassaemia major suffers from the disease throughout his life while a patient with thalassaemia intermedia can get thalassaemia major any time. A thalassaemia minor leads a normal life but is a carrier and can pass on the disease to his or her child. When two carriers of the Thalassemia gene (Thalassemia carriers) marry, in every pregnancy there will be 25% chance of Thalassemia Major Child, 25% of normal healthy child and 50% of Thalassemia carrier.
What are Signs/ Symptoms? There are several types of thalassemia. The signs and symptoms you have depend on the type and severity of your condition. Thalassemia signs and symptoms can include:
- Fatigue
- Weakness
- Pale or yellowish skin
- Facial bone deformities
- Slow growth
- Abdominal swelling
- Dark urine
Some babies show signs and symptoms of thalassemia around 4-6 months of age ; others develop them during the first two years of life.
Diagnosis: If you have minor or no symptoms, Doctor may suspect thalassemia based on the results of a routine blood test. Other types of thalassemia cause more severe symptoms that can be found earlier in life, usually before a child is 2 years old.To determine whether you or your child have thalassemia, your provider may ask about your risk factors, including your family’s and your medical history. Your provider might also order blood or genetic tests.
Blood and genetic tests
Your provider may order the following tests to determine whether you or your child have thalassemia:
- Complete blood count (CBC)
- Special hemoglobin test – HB Electrophoresis.
- Genetic testing can help determine what specific type of thalassemia you have.
What raises the risk of thalassemia?
Earlier it was be more likely to have thalassemia based on your family history and genetics and your race or ethnicity.
Family history and genetics
If your parents have mutations in the alpha globin or beta globin genes, or in other genes that affect the alpha or beta globin protein chains, then you can inherit thalassemia. If someone in your family has thalassemia, you may be a carrier. Carriers can pass the condition on to their children.
How is thalassemia treated?
Treatments for thalassemia depend on the type and how serious it is. If you are a carrier or have alpha or beta thalassemia trait, you likely have mild or no symptoms and may not need treatment.If you have a more serious thalassemia type like hemoglobin H disease, beta thalassemia intermedia, or beta thalassemia major you may experience moderate to serious anemia symptoms. You may need treatments such as blood transfusions, medicine, or a blood and bone marrow transplant.
Blood transfusions
Blood transfusions are the main way to treat moderate or severe thalassemia. This treatment gives you red blood cells with healthy hemoglobin.
During a blood transfusion, a needle is used to insert an intravenous (IV) line into one of your blood vessels. You receive healthy blood through this line. The procedure usually takes 1 to 4 hours. How often blood transfusions are needed depends on how serious your condition and symptoms are.
- Occasional blood transfusions may be needed for people who have hemoglobin H disease or beta thalassemia intermedia. Specifically, a transfusion may be needed when your body is under stress, such as during an infection, pregnancy, or surgery.
- Regular blood transfusions (every 3 to 4 weeks) may be needed for people who have beta thalassemia major. These transfusions help maintain healthy hemoglobin and red blood cell levels.
- Iron chelation therapy
- The hemoglobin in red blood cells is an iron-rich protein. Regular blood transfusions can cause iron buildup, or iron overload, which can lead to potentially life-threatening complications.
To prevent this, doctors use iron chelation therapy in people who receive regular blood transfusions to remove excess iron from the body.
A proper treatment of 30 kgs child can cost upto 2,00,000 rupees per annum and a curative approach Bone Marrow transplant can cost upto 10-15 lacs.
Can thalassemia be prevented?
Since thalassemia is caused by changes (mutations) in genes, there is no way to prevent it. People who do not know whether they carry a faulty gene that can cause thalassemia can ask their healthcare provider for a blood test.
Couples who are planning to have children and know that they are at risk of having a child with thalassemia may want to meet with a genetic counselor. A genetic counselor can answer questions about the risk and explain the choices that are available.
If you are pregnant and you or your partner has a family history of thalassemia, your provider may also recommend prenatal testing. Prenatal testing is done using a sample of amniotic fluid, the liquid in the sac surrounding a growing embryo, or of tissue taken from the placenta, the organ that attaches the umbilical cord to the mother’s womb. Testing before birth is safe and can be done as early as 8 to 10 weeks into the pregnancy.

